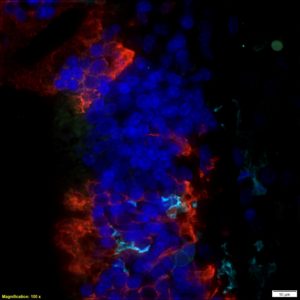
Emerging evidence from survivors of CoVID-19 increasingly points to effects in the brain, including encephalitis. Patients with underlying co-morbidity from disease or environmental exposures may be at greater risk for neurological manifestations of SARS-CoV2 infection, including dizziness, headache, impaired consciousness, acute cerebrovascular disease, ataxia and seizure. A systematic review of the effects of SARS-CoV2 and related viruses on cellular aging and stress pathways suggest strong similarities with pathways associated with neurodegeneration, including mitochondrial dysfunction, proteostasis, altered lipid metabolism and neuroinflammation. RNA viruses that present with severe peripheral inflammation, such as H1N1 influenza, western equine encephalitis virus (WEEV), West Nile virus (WNV), Japanese encephalitis virus (JEV) and St. Louis encephalitis virus, can cause a post-encephalitic form of PD in humans. They may also lead to aggregation of alpha-syn, suggesting an immunomodulatory role for this protein. Although the long-term neurological effects of CoVID-19 are not yet known, the high levels of inflammation induced by this virus suggest that infection with SARS-CoV2 could be a risk factor for development of neurodegenerative disease. To address this problem, we are investigating the neuroinflammatory effects of SARS-CoV-2 as well as translational therapeutic approaches involving small molecule immunomodulators that may prevent the entry of SARS-CoV-2 into cells.